Abstract
Introduction: Myeloid cells express PD1 and CTLA-4. Expression of these molecules is enhanced by azacitidine (AZA). Treatment of patients (pts) with nivolumab (Nivo) and anti-PD1 antibody or ipilimumab (Ipi) and anti-CTLA-4 antibody results in the upregulation of CTLA-4 in patients treated with Nivo and reversely of PD1 in patients treated with Ipi, potentially as a mechanism of evasion. In view of the activity of Nivo and Ipi in MDS (Garcia-Manero, ASH 2016), we hypothesized that dual combination of Nivo + Ipi with AZA could have significant activity in high risk MDS.
Methods: To study this, we designed a basket exploratory phase 2 trial of ICPI in MDS. Patients with MDS age 18 or older with adequate renal and hepatic function without history of autoimmune disorders were eligible. Patients were divided into front-line and HMA-failure cohorts. Front-line patients were treated with AZA 75mg/m2 iv daily days 1-5 of a 28 day cycle with Nivo 3 mg/kg iv on days 6 and 20 + Ipi 3 mg/kg iv on day 6. Patients with HMA failure where treated with Nivo 3 mg/kg iv on days 1 and 15 + Ipi 3 mg/kg iv on day 1 of a 28 day cycle. The study design allowed for AZA add-back after 6 cycles of therapy if there was no response or progression. The maximum size per cohort was 20 pts. The primary endpoint was to determine the safety of Nivo or Ipi as single agents or in combination with AZA. Secondary objectives included overall response rate (ORR) and assessment of biological activity. Responses were evaluated following the revised 2006 IWG criteria. The study included stopping rules for response and toxicity.
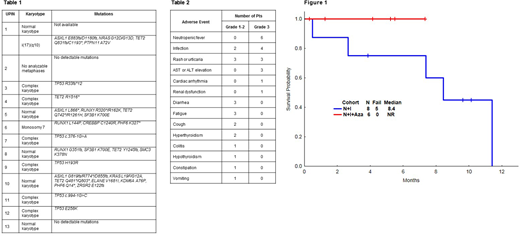
Results: The median follow up was 4.7 months [range 0-10 months]. From January 2017 to April 2018, 14 patients were treated, 6 pts on front-line cohort and 8 on HMA failure. The median age was 69 years [range 52-80]. A total of 4 (29%) pts had Int-1 risk, 6 (43%) had Int-2 and 4 (29%) had High risk by IPSS. Next generation sequencing on whole bone marrow extracted DNA was performed using a 28 gene panel in 5 pts and an 81-gene panel in 9 pts. Cytogenetic abnormalities and identified mutations are shown in Table 1. Median number of marrow blasts was 10 [range 1-16]. Median Hgb was 9.5g/dL [range 7.3-10.9 g/dL], median WBC was 1.5x109/L [range 0.9-4.7] and platelets was 29x109/L [range 8-117]. A total of 13 pts are evaluable for response at the time of analysis. A total of 3 (38%) pts in the HMA failure cohort received AZA after 6 cycles of therapy. The median number of cycles was 4 [range 1-10] with a median number of cycles to response of 3 [range 1-4]. The overall response rate was 50% (3/6) in the frontline cohort, all of them complete responses, and 29% (2/7) in the HMA failure cohort, including 1 complete response and 1 hematological improvement. Adverse events are shown in Table 2. Treatment with Ipi or NIvo had to be held due to rash in 2 pts, due to elevation of creatinine in 2 pts. Early mortality was observed in 1 patient and this was due to pneumonia complicated with respiratory failure and renal failure. The median overall survival is NR in the frontline cohort and is 8.4 months in the HMA failure cohort (Figure 1).
Conclusion: Preliminary results suggest double immune checkpoint inhibitor blockade with Ipi and Nivo in combination with AZA in the frontline setting, or in pts with HMA failure is associated with a tolerable safety profile and clinical activity.
Sasaki:Otsuka Pharmaceutical: Honoraria. Daver:Incyte: Research Funding; Novartis: Consultancy; Alexion: Consultancy; ARIAD: Research Funding; Daiichi-Sankyo: Research Funding; Otsuka: Consultancy; Novartis: Research Funding; Pfizer: Research Funding; Sunesis: Research Funding; Karyopharm: Consultancy; BMS: Research Funding; Incyte: Consultancy; Pfizer: Consultancy; Sunesis: Consultancy; Karyopharm: Research Funding; Kiromic: Research Funding; ImmunoGen: Consultancy. DiNardo:Abbvie: Honoraria; Celgene: Honoraria; Agios: Consultancy; Karyopharm: Honoraria; Medimmune: Honoraria; Bayer: Honoraria. Ravandi:Xencor: Research Funding; Xencor: Research Funding; Astellas Pharmaceuticals: Consultancy, Honoraria; Jazz: Honoraria; Amgen: Honoraria, Research Funding, Speakers Bureau; Sunesis: Honoraria; Seattle Genetics: Research Funding; Seattle Genetics: Research Funding; Amgen: Honoraria, Research Funding, Speakers Bureau; Sunesis: Honoraria; Astellas Pharmaceuticals: Consultancy, Honoraria; Abbvie: Research Funding; Orsenix: Honoraria; Jazz: Honoraria; Macrogenix: Honoraria, Research Funding; Orsenix: Honoraria; Abbvie: Research Funding; Bristol-Myers Squibb: Research Funding; Macrogenix: Honoraria, Research Funding; Bristol-Myers Squibb: Research Funding. Bose:Incyte Corporation: Honoraria, Research Funding; Astellas Pharmaceuticals: Research Funding; CTI BioPharma: Research Funding; Celgene Corporation: Honoraria, Research Funding; Constellation Pharmaceuticals: Research Funding; Pfizer, Inc.: Research Funding; Blueprint Medicines Corporation: Research Funding. Pemmaraju:plexxikon: Research Funding; daiichi sankyo: Research Funding; stemline: Consultancy, Honoraria, Research Funding; novartis: Research Funding; samus: Research Funding; celgene: Consultancy, Honoraria; cellectis: Research Funding; abbvie: Research Funding; SagerStrong Foundation: Research Funding; Affymetrix: Research Funding. Cortes:novartis: Research Funding. Kadia:Jazz: Consultancy, Research Funding; BMS: Research Funding; Abbvie: Consultancy; Novartis: Consultancy; Amgen: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Novartis: Consultancy; BMS: Research Funding; Celgene: Research Funding; Takeda: Consultancy; Celgene: Research Funding; Takeda: Consultancy; Abbvie: Consultancy; Jazz: Consultancy, Research Funding; Amgen: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding. Konopleva:Stemline Therapeutics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal